Inclusive ARFID Support
If eating feels overwhelming because of sensory sensitivities, fear of choking/vomiting, or a very limited range of “safe foods,” we’ll help you find a safer, steadier way forward – without shame, and with support around you.
- Comprehensive care: Personalised treatment plans tailored specifically for ARFID
- Specialist team: Evidence-based care with therapists trained in neurodiversity
- Caring environment: Compassionate support for sensory desensitisation to food
DO ANY OF THESE FEEL FAMILIAR?
Read through the list below – if any of this resonates, we can help you take the next safest step.
- Mealtimes feel stressful for you, or for someone you care about
- Avoiding foods because of texture, smell, taste, appearance, or temperature
- A very small range of “safe foods” (limited variety)
- Fear of choking, gagging, vomiting, or feeling unwell after eating
- Low interest in food or forgetting to eat
- Anxiety around eating with others, social events, school/university/work meals
- Worry about nutrition, energy, concentration, or health consequences
- ARFID traits overlapping with autism/ADHD sensory sensitivities or rigid routines
FINDING HOPE & STRENGTH IN YOUR RECOVERY
Are mealtimes a struggle for you or your loved one? Do you feel overwhelmed by the textures, tastes, or appearance of certain foods?
Unlike other eating disorders, ARFID is not associated with a distorted body image or fear of gaining weight. Instead, ARFID can involve:
- A lack of interest in eating
- Avoiding foods based on sensory characteristics (texture, smell, taste, appearance)
- Fear of negative consequences such as choking, gagging, or vomiting
Navigating ARFID can feel daunting – but you are not alone. Our compassionate team is here to support you step by step.
With our specialised ARFID support, you can experience:
THERAPY
A personalised approach that respects and understands your unique needs.
EXPERT TEAM
Integrated psychological, nutritional, and medical care where helpful.SUPPORT
A supportive environment that fosters trust and promotes positive food experiences.
GETTING STARTED
We’ll help you begin with what’s most pressing right now. Many people start with therapy to work with food-related fears, anxiety, rigidity, and the beliefs keeping the pattern stuck. We can then add structured nutrition guidance to support nutrition, energy, and gradual variety expansion at a realistic pace. If needed, we can also coordinate medical oversight so your physical health is prioritised.
Book a free 20-minute discovery call to talk it through — or email us if that feels easier.
BOOK A FREE 20-MINUTE DISCOVERY CALL
Choose a time for a confidential, no-pressure call.
We’ll listen, understand what’s been going on, and help you clarify the safest next step – including whether you’d benefit from therapy, nutrition support, or more specialist/integrated care.
Confidential • No pressure • Clear next steps
How It Works
Step 1 — Book a free call
Choose a time that works for you. It’s confidential and there’s no pressure to commit.
Step 2 — Free 20-minute discovery call
Tell us what’s been going on and what support you’re looking for. We’ll gently check what feels most important right now and whether we’re the right fit.
Step 3 — Clear next steps + clinician match
We’ll recommend the safest next step and keep the plan simple (therapy and/or nutrition first), then match you with the right clinician. If we think another service is safer or more appropriate, we’ll tell you.
Watch (0:57): Sarah from our Client Services team explains what happens on the free discovery call.
Prefer to enquire first? Send us a message
FEES & PRICING
Prefer to review pricing first? Explore our clear fees and package options.
ARFID THERAPY & TREATMENT
The sensory sensitivities and strong food aversions associated with ARFID can significantly impact quality of life and wellbeing. If you’re seeking a structured approach, our support can include:

THERAPY
Tailored therapy to work with underlying anxiety, food-related fears, and avoidance patterns – building safer coping strategies and confidence over time.

NUTRITION
Personalised guidance to meet nutritional needs while gradually expanding variety in a safe and supportive way (including fortified foods/supplements if needed).

MEDICAL (WHEN NEEDED)
Monitoring and coordination to ensure physical health is prioritised throughout the process.
Recovery can be transformative. It’s possible to reclaim your relationship with food and build a more fulfilling, balanced life.
MEET JAMES, OUR FOUNDER & CEO
James shares how we work with ARFID support at WeightMatters – and what a supportive first step can look like.
TRUSTED, CONFIDENTIAL SUPPORT
Many people tell us the hardest step is reaching out – these are a few words from clients about what it was like to be supported.
“ARFID explained what I’d been calling ‘picky eating’ … the sensory overwhelm and panic around unfamiliar foods. Going at my pace with small steps helped me widen my safe foods and feel less anxious around meals.”
– Daniel
“I reached out… and for the first time, I felt hope… With the option for online sessions, I was able to access support from afar… The environment was incredibly supportive.”
– Rachel
“For the first time, I felt properly listened to and properly understood.”
– Karen
“I avoided eating with others because I felt embarrassed and stressed. Having someone who understood ARFID made it feel manageable, not shameful … I’m eating more consistently now and feel much calmer in social situations.”
– Constance
“The ‘pressure to just try it’ never worked for me. This approach was gentle and practical, with tiny experiments I could actually do. I’ve built confidence with food and don’t feel broken anymore … I feel understood.”
– Helena
Selected feedback from WeightMatters clients. Individual experiences vary.
ALEX – DOES THIS SOUND FAMILIAR? When food becomes the enemy: navigating life with ARFID.
Alex’s story is one many people recognise – a small range of “safe foods,” intense sensory discomfort, and growing anxiety around eating.
- Sensory sensitivity: textures, smells, tastes, or appearance making foods feel unbearable
- Safe foods only: a narrow range of foods that feel predictable and manageable
- Fear of consequences: worry about choking, gagging, vomiting, or feeling unwell
- Social impact: avoiding meals with friends, dates, university/work gatherings
- Energy and focus: nutrition gaps affecting concentration, fatigue, or wellbeing
- Readiness for support: wanting a plan that feels respectful, calm, and achievable
ADHD, NEURODIVERSITY & ARFID – UNDERSTANDING THE INTERPLAY
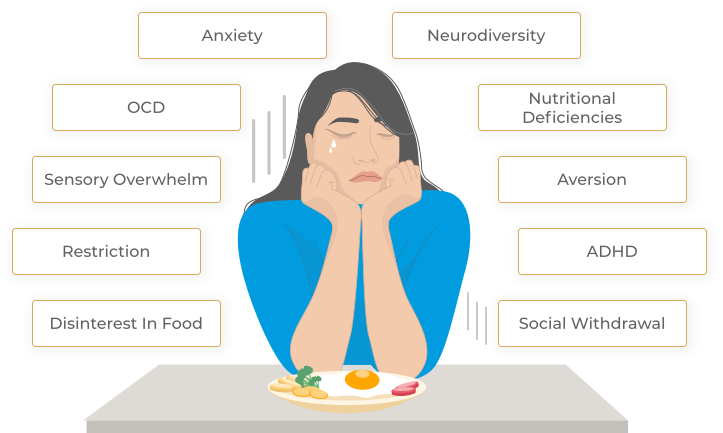
The overlap between neurodiversity presentations (including ADHD and autism) and ARFID can be significant. For many people, ARFID is shaped by:
- Sensory processing differences: texture/smell/taste sensitivity and overwhelm
- Anxiety and rigidity: fear of uncertainty, difficulty with change, “rules” around safe foods
- Co-existing mental health: anxiety, OCD traits, trauma, or low mood that intensify food fear
- Communication and social challenges: difficulty negotiating meals or expressing food needs
- Developmental and feeding history: long-term patterns that persist into adulthood
Our approach is tailored to sensory and cognitive differences, with compassion and clarity.
FAQs
If you’re not sure what’s going on or what to do next, these answers may help — and you can always book a free discovery call to talk it through.
ARFID is an eating disorder where someone restricts the amount they eat and/or avoids many foods – often due to sensory sensitivities, low interest in eating, or fear of negative consequences like choking or vomiting. ARFID is not primarily about weight loss or body image.
ARFID is more than typical picky eating when it significantly impacts nutrition, health, energy, growth (in young people), or daily life – and causes distress or avoidance.
Yes. ARFID can affect children, teenagers, and adults. Adults may access support through specialist eating disorder services, general mental health services, and/or dietetic support. Private support can also help you start sooner.
Many people identify with one or more patterns:
- Sensory-based avoidance (texture/smell/taste/appearance)
- Fear of consequences (choking, vomiting, pain, nausea)
- Low interest in eating (low appetite/forgetting to eat)
ARFID support is usually gradual and collaborative. It can include psychoeducation, anxiety management, CBT-style approaches, sensory strategies, and gentle food exposure/expansion at a pace that feels tolerable – alongside nutritional planning to meet needs safely.
Yes. Many people with ARFID are neurodivergent or have sensory processing differences. Our approach can be adapted for sensory needs, anxiety, routines, and cognitive style.
Many people benefit from dietetic support to ensure nutritional needs are met, plan safe expansions, and reduce nutritional risk – especially if variety is very limited. We’ll recommend a safe starting point for you.
It’s a confidential, no-pressure conversation. We’ll ask what’s been happening (safe foods, sensory triggers, fears, impact on life), what you’ve tried, and what you want to change. We’ll then suggest clear next steps – including whether therapy, nutrition support, or medical input is appropriate.
You can still book a call. We’ll talk through what’s happening and advise on safe next steps and the most appropriate support route.
Yes. Your enquiry and sessions are confidential. We’ll explain how confidentiality works and when we might need to share information for safety reasons (for example, if there’s immediate risk). In day-to-day terms: you can speak openly and safely, and we’ll be clear about boundarie
CLINICAL STANDARDS & HOW WE WORK
We follow clear clinical standards so you know what to expect – from confidentiality and consent, to safe next steps and appropriate signposting.
How We Work
- Clinician-led, evidence-informed support tailored to your situation
- Confidential, respectful care with clear boundaries and consent-led communication
- Integrated support where helpful (therapy, nutrition, and medical oversight when needed)
- Collaborative care if appropriate – we can liaise with your GP/consultant, with your permission
- Appropriate onward signposting if you need a different type of support or a higher level of care
- Privacy and data protection – see our Privacy Policy
Safety Note – If you’re feeling at immediate risk of harm or having suicidal thoughts, please seek urgent support via 999/A&E, 111, or your GP.
We follow internal clinical governance and safeguarding standards; details are available on request.
Content owner: James Lamper, Clinical Director
Clinically reviewed by: Dr Natascha Van Zyl, Director of Talking Therapies
Last reviewed: February 2026
RELATED SERVICES
Explore these support options we may recommend as part of your care.
Therapy • Dietitian Support • Nutritional Therapy • Psychiatry • Healing Disordered Eating
NEURODIVERSITY POSITIVE PRACTICE
We aim to create a space where every brain is understood and respected – including sensory sensitivities, anxiety, and rigid patterns that can overlap with eating difficulties.
IF IT FEELS EASIER, EMAIL US
Have a question before booking? Leave your details and our Client Services team will reply with a personalised response. Confidential and no pressure.
