Diabetes Care
- Weight Loss: Personalised Plan To Support Lasting Weight Loss
- Targeted Therapy: Psychological Interventions To Challenge Self Sabotage
- Integrated Care: Blending Medical, Psychological & Nutritional Support
DIABETES CARE
Take Control Of Your Health: Navigate Your Path To Wellness
At WeightMatters, we understand that managing diabetes, when complicated with weight struggles or an eating disorder, involves more than just physical health – it’s about nurturing the whole person.
Our approach is centered around providing you with the tools, support, and encouragement you need to thrive. We recognize the emotional challenges and social pressures that can accompany these conditions, and we are here to guide you through every step of your journey.
Comprehensive Multidisciplinary Care
Our dedicated team of professionals, includes endocrinologists, dietitians, psychologists, and exercise specialists. This multidisciplinary approach ensures you receive holistic care that addresses both the medical and emotional aspects of your wellbeing.

Motivational Support & Counselling
We provide personalised motivational support aimed at empowering you to make positive lifestyle changes. Our counsellors help you set realistic goals, build resilience, and maintain a positive outlook on your health journey.

Customised Nutrition & Exercise Plans
We create tailored nutrition and exercise plans to fit your lifestyle and preferences. These plans are designed to optimize your health and make sustainable changes that enhance your quality of life.

Emotional Wellbeing & Psychological Support
Dealing with diabetes can bring emotional struggles that can complicate your relationship with food and your body. Our experienced therapists offer compassionate support and coping strategies to help you manage these challenges.
We are committed to helping you navigate your experience of diabetes and how it personally affects your mental health, physical health, and your relationship with food, eating and your body.
Our team is committed to guiding you every step of the way, nurturing weight management, holistic wellness and personal growth.
TAKE CONTROL OF YOUR HEALTH TODAY – WE ARE HERE TO HELP
Struggling with weight and eating challenges? You don’t have to face it alone.
Our compassionate team is ready to listen, support, and guide you toward a healthier, happier life.
Book your free call now and take the first step.
MEET PAUL, HEAR HIS STORY
Paul shares his experience of weight loss and learning how to manage his health.
Jane – Do You Resonate With Her Story?
Jane, a 38-year-old woman, has battled with her weight for most of her life. She frequently found herself resorting to emotional eating during stressful and challenging times, using food as a coping mechanism.
When she was diagnosed with type 2 diabetes a year ago, the news came as a shock. She felt overwhelmed by the implications on her health and the urgent need to change her lifestyle.
The healthcare team at the NHS was supportive and provided her with invaluable general guidance on managing diabetes through medication and information. However, the realisation quickly set in that the resources for personalised therapy focusing on her underlying issues of emotional eating were limited.
Recognizing the gap in her care, Jane began looking for more specialised support that could address her diabetes management while delving deeper into her psychological challenges with food.
She understood that her journey required not just a medical plan, but also a comprehensive approach that would equip her with healthier coping strategies.
Jane sought out a specialized clinic that offered both the ongoing medical care necessary for her diabetes and a multifaceted support system featuring psychotherapy to help her unpack and tackle her emotional eating habits.
This clinic also promised nutritional coaching, pivotal for helping her establish new eating patterns that aligned with her health goals.
With her sights set on this integrated plan, Jane started working with the specialised team comprising endocrinologists, therapists, and nutritionists who tailored her treatment to her unique needs.
Through therapy sessions, she began to understand the emotional triggers that led to her eating habits and was given tools to address these feelings in constructive ways.
The nutritional coaching provided her not only with meal plans conducive to her condition, but also taught her the importance of a balanced diet that fits within her lifestyle.
Similarly, ongoing diabetes management ensured her health was monitored closely, allowing Jane to feel empowered and supported on her path toward personal transformation and healthier living.
Type 1 Challenges
People with Type 1 diabetes can struggle with their condition, related to their weight, eating behaviour, physical and mental health.
Psychological & Emotional Challenges
- The constant monitoring of blood sugar levels, meal planning, and insulin administration can contribute to stress, anxiety, and even burnout.
- Concerns about food becoming an obsessive focus, which can inadvertently lead to disordered eating behaviors.
- The emotional toll of weight management and body image issues often exacerbates these challenges
Balancing Diabetes Management with Weight Control
- Finding a balance between managing diabetes effectively and controlling weight.
- Difficulties of achieving optimal blood glucose control while trying to lose or maintain weight, as insulin can sometimes promote weight gain.
- Challenges with determining appropriate carbohydrate intake and balancing their diet, which can lead to feelings of helplessness or confusion.
Access to Resources and Support
- Inadequate access to appropriate healthcare resources and support systems
- Lack of specialised care addressing the intersection of diabetes, obesity, and eating disorders.
- Desire for more comprehensive, multi-disciplinary approaches that offer psychological support, nutritional counseling, and medical advice tailored to their specific needs.
- Many feel they have to manage complex aspects of their health on their own.
Diabulimia
Diabulimia is often driven by body image issues and a desire for thinness, combined with the mental health challenges associated with living with a chronic condition.
People with Type 1 diabetes rely on insulin to manage their blood glucose levels. In diabulimia, individuals reduce or withhold the insulin necessary for glucose uptake to cause the body to burn fat and muscle for energy, potentially leading to weight loss.
Type 2 Challenges
We often meet clients with Type 2 diabetes who face a variety of challenges related to managing their condition, controlling their weight, and their mental health. Here are some of the common struggles they face:
Managing Blood Sugar Levels
- Complexity of Management – Clients with Type 2 diabetes must monitor their blood sugar regularly and adjust their diet, physical activity, and potentially medication or insulin use accordingly. This ongoing effort can be overwhelming and challenging.
- Dietary Changes – Dietary management often requires significant lifestyle adjustments, such as reducing carbohydrate intake, controlling portion sizes, and making healthier food choices. Many people find these changes difficult to maintain consistently, particularly if they lack access to nutritious food options or face dietary restrictions they find culturally or personally unappealing.
Struggles With Weight Control
- Insulin Resistance – A hallmark of Type 2 diabetes, insulin resistance can make weight loss more difficult. Clients often experience challenges in losing weight, which is typically recommended for improving insulin sensitivity.
- Weight Gain from Medications – Some diabetes medications, including insulin, can promote weight gain, leading to a cycle that makes managing both diabetes and weight increasingly complex.
- Emotional Eating – Emotional stress, sometimes related to the diabetes diagnosis or its management, can lead to emotional or stress eating, further complicating weight management efforts.
Psychological & Emotional Factors
- Mental Health – The burden of managing diabetes can lead to stress, anxiety, or depression. These mental health issues can, in turn, impact a client’s motivation and ability to adhere to treatment plans.
- Body Image Issues – Concerns about body weight and body image can sometimes lead to unhealthy eating behaviors or disordered eating.
Insulin Management
- Manipulation of Insulin – Some individuals with Type 2 diabetes, especially those who transfer to insulin therapy, may underuse insulin to avoid weight gain. This practice can lead to poor blood sugar control and a host of subsequent health complications.
- Seeking Quick Fixes – The pressure to maintain or reduce weight can push individuals toward harmful behaviors, risking long-term health for short-term goals.
Lack of Resources & Support
- Access to Healthcare – Quality care, education, and support for comprehensive diabetes management can be limited, particularly in underserved communities. This lack of access can leave individuals feeling unsupported.
- Education Gaps – Insufficient information about diabetes management and healthy lifestyle changes may impede patients’ ability to effectively manage their conditions.
Overall, the struggles with Type 2 diabetes, weight control, and related challenges highlight a need for comprehensive care that includes medical treatment, dietary advice, psychological support, and accessible resources to empower individuals in managing their health effectively.
We can create a tailored programme to support your personal challenges living with diabetes. Call our team today, and find out how we can support you.
WEIGHT LOSS
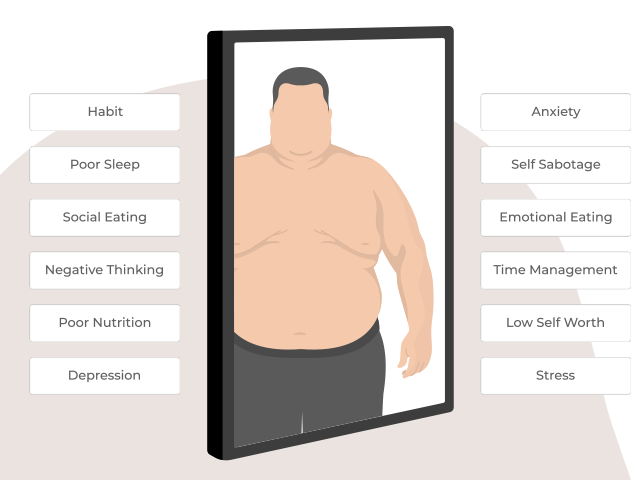
Your struggle with weight is deeply personal to you, and consists of multiple psychological, emotional and social factors. Now is the time to change your story.
DIABETES TREATMENT
Managing diabetes, especially when complicated by conditions such as obesity and other health conditions, requires a holistic approach, to deliver coordinated, client-centered care.
Our expert multi-disciplinary team works collaboratively to support you, bringing together skills from therapy, nutrition, psychiatry, and general medicine, all working together to ensure you receive holistic and tailored support.

THERAPY
Cognitive and behavioral support helping you develop healthier thought patterns and coping strategies to enhance diabetes management.

NUTRITION
Personalised nutrition plans tailored to your lifestyle and health goals to maintain stable blood glucose levels.

PSYCHIATRY
Addresses coexisting mental health issues to facilitate balanced diabetes management through therapy and medication if necessary.

PRIVATE GP
Integrated medical oversight provides regular evaluations and coordinated care to optimise insulin management and prevent complications.
We are committed to empowering you on your diabetes management journey. Our dedicated team provides a supportive environment for achieving a balanced, healthy lifestyle.
Are you ready to get started on your path to improved health? Contact our team today and let us get you started on a treatment plan to help you achieve your health goals.
It’s Time To Heal.
Therapy
Our therapists use a range of techniques and interventions to help individuals who have a complex relationship with diabetes. These approaches are tailored to address the intertwined physical and psychological aspects impacting their wellbeing.
1. Cognitive Behavioral Therapy (CBT) – This helps clients identify and change negative thought patterns and behaviors related to eating, body image, and diabetes management.
2. Motivational Interviewing (MI) – This client-centered technique is designed to enhance motivation to change diabetes-related behaviors by exploring and resolving ambivalence.
3. Mindfulness-Based Interventions – Techniques such as mindfulness-based stress reduction (MBSR) or mindfulness-based cognitive therapy (MBCT) can help individuals become more aware of their eating habits and body image issues, promoting more mindful eating and improved self-acceptance.
4. Acceptance & Commitment Therapy (ACT) – This approach encourages acceptance of the emotional distress associated with diabetes and body image issues while committing to actions that align with personal values.
5. Dialectical Behavior Therapy (DBT) – Originally developed for emotional regulation, DBT can help individuals manage stress and emotional eating, fostering a healthier relationship with food and their bodies.
6. Body Image Restructuring Therapy – Techniques that promote positive body image and self-acceptance, such as challenging societal norms around body weight and fostering a more realistic body perception.
7. Behavioural Activation – Encouraging engagement in behaviours that improve mood and increase positive interactions, which can contribute to better diabetes management and healthier lifestyle choices.
8. Self-Compassion Therapy – Fostering self-kindness and understanding rather than self-criticism, which can be detrimental to both mental well-being and diabetes management.
Each of these approaches is chosen and personalised to fit your unique needs and circumstances, ensuring a comprehensive curated treatment strategy.
We often combine these techniques with medical management, which can significantly enhance overall health outcomes for individuals grappling with these intertwined physical and psychological challenges of diabetes.
Nutrition
Dietitians and nutritional therapists employ various techniques and interventions to support individuals managing complex relationships with diabetes, obesity, and their body.
These approaches are designed to promote healthier eating habits, improved body image, and effective diabetes management. Here are some specific techniques they might use:
1. Personalised Nutrition Counselling – Tailoring nutritional advice to align with the individual’s specific health needs, diabetes management goals, lifestyle, and cultural preferences.
2. Medical Nutrition Therapy (MNT) – A therapeutic approach to treating chronic conditions, including creating individualised meal plans that focus on proper carbohydrate counting and portion control to manage blood glucose levels.
3. Mindful Eating Practices – Encouraging awareness and appreciation of food through mindful eating techniques to reduce overeating, emotional eating, and improve body image.
4. Intuitive Eating – Teaching clients to listen to their body’s hunger and fullness cues, helping them to cultivate a healthier relationship with food and combat emotional eating.
5. Behavior Modification Plans – Assisting clients in identifying triggers for unhealthy eating patterns and developing strategies for behavior change, such as keeping a food journal, setting realistic goals, and celebrating progress.
6. Cultural Sensitivity & Adaptation – Creating nutrition plans that respect and incorporate the individual’s cultural background and familial food practices to promote sustainability and acceptance.
7. Support for Weight Neutral Approaches – Encouraging a focus on health-promoting behaviors regardless of weight change, which can improve body image and reduce stress around food choices.
8. Diabetes Self-Management Education (DSME) – Providing comprehensive education to help individuals build the skills required for effective diabetes management, including blood glucose monitoring and understanding medication impacts.
Each of these strategies is adapted to your personal goals and challenges, ensuring a comprehensive, empathetic approach to improving health outcomes.
Working both independently and as part of a broader healthcare team, dietitians and nutritional therapists play a crucial role in addressing the complex interplay of diabetes, obesity, and other health conditions.
Medical
Our medical team consists of a private GP, endocrinologist, and bariatric surgeon who can offer a range of techniques and interventions to support individuals dealing with diabetes, obesity, and comorbid health conditions.
These healthcare professionals focus on medical management, surgical options, and personalised care plans that address both the physiological and psychological aspects of these conditions. Here are some specific interventions they might use:
PRIVATE GP
- Comprehensive Health Assessments – Regular monitoring of blood glucose, blood pressure, cholesterol levels, and BMI to track health progress and adjust treatment plans accordingly.
- Medication Management – Prescribing and managing medications to control blood sugar levels, improve insulin sensitivity, or aid in weight loss, such as metformin or GLP-1 receptor agonists.
ENDOCRINOLOGIST
- Advanced Hormonal Assessments – Evaluating and managing complex hormonal imbalances that may contribute to obesity and diabetes, such as thyroid function or adrenal disorders.
- Insulin Therapy Optimization – Fine-tuning insulin regimens to achieve optimal blood sugar control, accommodating the person’s lifestyle and dietary habits.
- Continuous Glucose Monitoring (CGM) Deployment – Implementing CGM systems to provide real-time glucose readings and help patients and their healthcare team better manage insulin dosing and food intake.
- Risk Factor Modification – Addressing other health risks, such as cardiovascular disease, by managing lipid profiles and blood pressure as part of comprehensive diabetes and obesity management.
BARIATRIC SURGEON
- Bariatric Surgery Options – Offering surgical interventions such as gastric bypass, sleeve gastrectomy, or a mini gastric bypass to aid significant weight loss and improve metabolic health.
- Pre-Surgical Counseling & Preparation – Ensuring the patient is fully informed about surgery risks, benefits, and required lifestyle changes post-surgery through detailed counseling.
- Multi-Disciplinary Team (MDT) – Collaborating with the endocrinologist and bariatric dietitian to ensure the patient receives adequate nutrition following surgical procedures and to prevent complications like nutrient deficiencies.
Each type of healthcare professional contributes uniquely to the multidisciplinary care of individuals with diabetes and obesity. By working collaboratively, our team aim to deliver comprehensive, patient-centered care tailored to managing these complex conditions effectively.
Get help today
Start your healing journey
Contact us
Take the first step, reach out and talk to us.
You can refer yourself for treatment, or get a referral from a healthcare professional.
Call us on 020 7622 7727, email us a question or book a call.
Time to start
Share your experience
Our friendly and experienced team will listen carefully to your reason for contacting us.
They will ask some questions and match you to the service and practitioner that best fits your needs.
Time to ask
Your assessment
Your journey starts with your initial assessment session.
Your practitioner will explore your current situation, ask about your change goals, and create your bespoke treatment plan.
Time to understand
Treatment, healing & recovery
When you have agreed your treatment plan, you will meet with your practitioner / team to support your recovery.
We will support you every step of the way as you create a healthier relationship with weight, food and your body.
Time to heal
GETTING STARTED – DIABETES TREATMENT
We believe it is important for clients to begin their diabetes treatment by focusing on the area most impacting them.
Some might initially start with therapy to address psychological and emotional factors, while others might opt to see a nutritionist first to establish a healthier eating structure.
As you progress forward through your treatment with us, additional services can be seamlessly integrated into your plan.
Our Healing Disordered Eating: Rebalance programme allows you to blend both our psychology and nutrition services for effective treatment for disordered eating.
Our Holistic Weight Loss: Reframe programme allows you to blend both our psychology and nutrition services, and our Weight Loss Medication packages provide support with both our medical and nutrition teams, to support healthy weight loss.
Let us support you with our effective multi-disciplinary team (MDT) approach for effective diabetes treatment. Now is the time to understand your eating behaviour, and develop a programme that transforms your life.
It is time to feel hopeful, heal, and start your journey to recovery.
Call us now, or book a free assessment call with our friendly client services team, who will answer any questions you have.
IT’S TIME TO START YOUR HEALING JOURNEY
You can discover our clear pricing structure.
SERVICES WE RECOMMEND FOR DIABETES TREATMENT
Here are the WeightMatters services we recommend for effective diabetes treatment.
IF IT FEELS MORE COMFORTABLE, EMAIL US
Do you have a question about our treatment and support?
Leave your details below, and we will come back to you with a personalised response.
